Executive Summary
The Faculty of Public Health (FPH) is committed to addressing inequities in pay and terms and conditions (T&Cs) among specialist public health consultants. Despite undergoing identical training, acquiring the same competencies, and performing equivalent roles, registrars and consultants from multi-professional backgrounds often receive significantly lower pay and benefits than their medically qualified counterparts. This longstanding disparity has widened over time, exacerbating workforce challenges and creating an unfair labour market.
Unlike most medical specialties, public health is a multi-professional field where specialists can come from both medical and non-medical backgrounds. However, only medical consultants benefit from national medical T&Cs, while those from non-medical backgrounds are frequently placed on Agenda for Change (AfC) contracts, often at Band 8d. Moreover, many public health consultants are employed outside the NHS, particularly in English local authorities, where salary disparities are more pronounced and funding for national pay awards is inconsistent.
FPH’s strategy advocates for an optimal solution where all public health consultants receive equitable contracts aligned with those of other medical specialists. Key recommendations include standardizing employment contracts, ensuring continuity of service across employers, and supporting regulatory consistency. However, recognising the challenges of full implementation, amelioration actions—such as reducing pay differentials, harmonizing T&Cs, and advocating for improved recognition—are also proposed.
To achieve these goals, FPH will engage with government, employers, and trade unions while exploring regulatory opportunities. Addressing these inequities is essential to maintaining a sustainable, diverse, and highly skilled public health workforce.
Introduction
Public health is a medical specialty. It is a unique medical specialty in that it allows entry to the specialty by people from a medical background (doctors) and by people with multi-professional backgrounds. Both groups enter the public health training programme the same way, go through the same training pathway (usually between 5-6 years in duration) and acquire the same skills and competencies. All registrars (trainees) will gain a certificate of completion of training (CCT) when they finish their training. This allows them to join one of the specialist registers, which is essential to apply for and be eligible for specialist (consultant) posts in public health. Again, this is consistent with all other medical specialties.
This paper will look primarily at the disparities in terms and conditions between those in the senior workforce (consultants/specialists). However, it is worth noting that disparities exist and are embedded in the career pathway of public health consultants well before specialist registration. In relation to public health training:
- Over the course of a typical five-year training pathway, the base pay of public health registrars from backgrounds other than medicine is over £32,000 less than colleagues from medical backgrounds.
- Those entering training from a medical background have at least two years previous NHS service recognised for the purposes of reckonable service. Those from multi-professional (‘non-medical’) backgrounds typically do not have their previous work history recognised, despite having eligibility criteria requiring a minimum of two years of experience in a role ‘relevant to population health practice’. This has significant implications for annual leave, sick pay and maternity pay entitlements.
At a more senior level, once on one of the specialist registers and practicing public health at consultant/specialist level, people who have successfully completed an identical specialist training programme and are working according to an identical job description are being rewarded with significantly different pay and terms and conditions (T&Cs). This is the reality for many consultants in public health. If a consultant comes from a medical background and is on medical terms and conditions of service, they will enjoy significantly better pay and T&Cs than identically trained people, doing the same job, who come from multi-professional backgrounds and who will often be on Agenda for Change (AfC) contracts. This clear inequity is not new and has been present for many years; however, pay differentials are widening and the adverse effect this is having on the public health workforce is increasing.
It has been accepted for many years that consultants from all medical specialties should be on the same contract. Therefore, as would be anticipated, medically qualified public health consultants who are on medical consultant T&Cs have very similar contracts to colleagues from any other medical specialty. However, whilst the vast majority of medical consultants across all specialties work for employers who offer medical T&Cs as a routine, in public health some of the major employers of consultants e.g. English local authorities rarely offer medical consultant T&Cs. As a result, the doctors working for these employers earn far less than their colleagues who have medical contracts with other employers. This clear inequity distorts the public health workforce market as many medically qualified public health consultants will not apply for posts with organisations who do not offer medical consultant salaries.
Public health is also unusual as a medical specialty in that the majority of consultants are not employed by the NHS. These non-NHS employers usually are not fully funded to meet the consequences of national pay awards. This is a reason why even amongst non-medically qualified public health consultants, pay in these non-NHS organisations e.g. English local authorities, is often less than offered under Agenda for Change.
Although the Faculty is not an organisation primarily concerned with pay and T&Cs, it has a clear role in supporting the wellbeing of its members and in ensuring parity of esteem for the specialist workforce and assisting in the development of a healthy, fair and balanced labour market. This strategy proposes ways in which these unreasonable and unjustifiable inequities in the system can be addressed.
Background
Historically, public health consultants all came from a medical background and a large majority were employed by the NHS. These consultants had virtually identical terms and conditions of service to consultants from other medical specialties. All these consultants were regulated by the GMC.
At different times over the past few decades, the Four Nations of the United Kingdom decided that public health should become a ‘medical specialty with equivalent training open to persons whose initial professional background was non-medical’. De facto, public health became a multi-professional specialty and benefits enormously from the richness and diversity that multi-professionalism provides. In the four UK nations, the number and type of employers of public health consultants has gradually increased. The widest number of employers is in England, with local authorities, UKHSA, OHID, the NHS and universities all employing significant numbers of consultants. In Wales, Scotland and Northern Ireland, the NHS remains the largest employer of consultants.
Although identical specialist training in public health was introduced, irrespective of initial professional background, the pay and T&Cs of consultants was never regularised; doctors continued on medical T&Cs, whilst consultants from multi-professional backgrounds received lower pay and had different T&CS. Typically, consultants from multi-professional backgrounds were placed on Band 8d in the Agenda for Change scheme. A large majority of consultants from multi-professional backgrounds were registered and regulated by the UKPHR, but dentists who successfully completed specialist training in dental public health under the auspices of the Royal College of Surgeons were regulated by the GDC.
In England, a major reorganisation of the public health system was introduced in 2013, resulting in the transfer of many public health consultants to local authorities. Although it was recommended that continuity of service would be recognised when staff moved between NHS and non-NHS employers, and that pay should remain equivalent to that in the NHS, local authorities effectively had the freedom to ignore this advice. It is now the case that local authorities rarely offer doctors medical contracts and there is some evidence that councils may offer lower salaries than those covered by the NHS Agenda for Change scheme. Continuity of service is usually recognised.
In Wales, following a recent evaluation of public health consultant posts, it was agreed that the minimum banding for consultants on the AfC scheme should be Band 9. This has led to salaries in Wales being higher than in England and Scotland, although doctors in Wales still earn on average much more over their professional lifetimes than their consultant colleagues from multi-professional backgrounds.
The pay differential between consultants medical and from multi-professional backgrounds is increasing. Doctors also have access to national clinical impact awards (formerly ACCEA) or their equivalent, and these can be significant (up to £40,000 per year for five years). There are also non-pay differences in T&CS such as out-of-hours payments and weekly contracted hours.
Numbers of consultants and registration summary
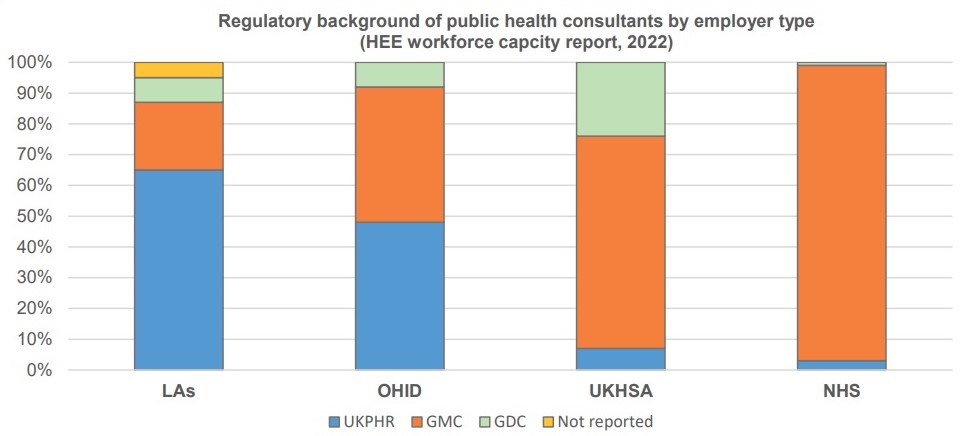
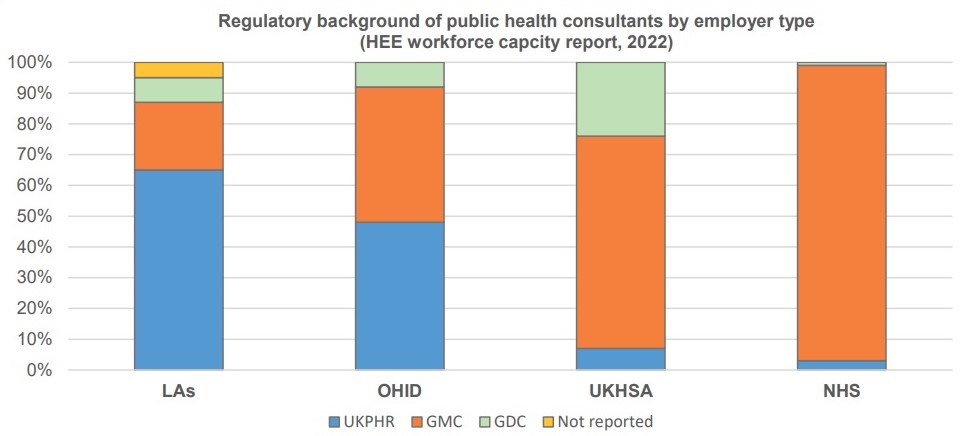
The last analysis of capacity and workforce across England was carried out by Health Education England (HEE) in 2022. A workforce census is due to be conducted by NHS England WT&E in the latter part of 2025.
From the findings in 2022, the main employers of public health consultants were:
- Local authorities (LAs): 595 (48 per cent)
- United Kingdom Health Security Agency (UKHSA): 139 (19 per cent)
- Office for Health improvement and Disparities (OHID): 53 (4 per cent)
- NHS: 206 (17 per cent)
- Higher educational institutes (HEIs): 145 (12 per cent).
A vision for change: what would good look like?
A suitable solution to this issue has long been sought by the Faculty and by public health professionals and its parameters are set out below. However, the desire to achieve an equitable solution has proved challenging and therefore a realistic strategy needs to consider steps which can both ameliorate the inequalities in the situation as well as actions to achieve the optimal solution.
The optimal solution
- All public health consultants have the same contract, irrespective of professional background, a contract which essentially is one with similar terms and conditions to consultants in other specialties.
- Continuity of service is recognised for movements between different employers, within and outside the NHS.
- All public health consultants are subject to the same regulations.
- All employers are obliged to offer the same contract to registered public health specialists.
- The government commits to fully funding all employers in the public sector, including local authorities. The Department of Health and Social Care would meet national pay awards and allow the setting up of additional agreed national public health training places.
This solution would be equitable, would improve recruitment and retention of staff, would facilitate a flexible specialist workforce and would reduce the current frustrations amongst senior public health staff. This would be worth the additional salary costs that would be consequent upon adoring this option.
Amelioration actions would reduce some of the inequity in the system. Some desirable outcomes of amelioration would be:
- A significant reduction in pay differences.
- Harmonisation of some T&CS.
- Recognition of continuity of service.
A FPH strategic approach
Given this vision, the Faculty of Public Health aims to achieve equitable pay, terms, and conditions for all public health consultants, regardless of their professional background. This will ensure fairness, promote workforce sustainability, and reinforce the recognition of public health as a medical specialty.
Specific objectives are to:
- Engage with our members, employers and relevant stakeholders to document and monitor the nature and range of the existing and emerging disparities and to monitor their impact on the current and future public health workforce.
- Engage public health stakeholders and policymakers to advocate for standardisation of public health consultant contracts, securing three formal policy discussions and publishing a policy position papers on this issue.
- Work with major employers to harmonize consultant salaries, securing commitments from at least 50% of local authorities to re-evaluate salary structures by 2026.
- Communication and engagement with our members about our work and progress in addressing this issue, recognising the collaborative nature of this approach.
Potential actions
Whilst this is a Faculty strategy, not all potential actions would be appropriate lead roles for a charity and professional membership body. Some actions would be best led by trade unions representing Faculty members, as one of the primary roles of trade unions is to improve the pay and T&CS of its members.
Action with government
The FPH President will write to the Public Health Minister summarising the major inequities in the system and how that is affecting the labour market for specialist public health staff. The Minister will be asked to implement the steps needed to achieve the aforementioned ‘optimal’ solution. If dialogue with the Minister indicates that s/he is only willing to consider amelioration actions, the Faculty will discuss these options.
Unions representing the specialist public health workforce (BMA, Unison etc.) will be urged to make similar representations to the Governments in the Four Nations.
Action with employers
The Faculty will continue to urge all major employers of specialist public health staff to regrade their consultant posts to narrow the gap between the salaries of consultants on medical T&CS and other consultants. For example, staff who are appointed under Agenda for Change T&CS should be offered at least Band 9 funding.
The Faculty will ask major employers to use their discretion to:
- Recognise continuity of service.
- Allow staff to continue on NHS pension arrangements.
- Agree local harmonisation of T&Cs e.g. re OOH arrangements.
The Faculty will urge unions to have similar dialogue with employers. The Faculty will maintain its view that all NHS organisations must advertise consultant posts to all suitably qualified practitioners and offer medical T&CS to public health doctors. The idea of some NHS organisations only offering AfC salaries is not accepted.
Some Faculty members have suggested that they take out grievance actions against their employer. Such action should be discussed with the relevant union.
Legal action
The Faculty, along with the BMA, has obtained a legal view that there is not a realistic chance of success in pursuing an equal pay claim under the existing legislation.
Regulatory action
It has been a recognised FPH policy for several years that all public health specialists (consultants) should be registered with a statutory regulator. As noted above, this is not currently the case with the public health consultant workforce split in terms of regulation between the statutory regulators: the General Medical Council (GMC), with a much smaller number registered with the General Dental Council (GDC) and the non-statutory UK Public Health Register.
While the role of the GMC has been expanded over recent years to cover some non-medically qualified staff, such as physician associates, it remains the case that the public health workforce is split between statutory and non-statutory regulators. Harmonisation of this position would demonstrate that all public health consultants had parity of esteem with other medical specialty consultants. It would not in itself lead to changes in public health contracts, but it would strengthen the moral case that all public health consultants should enjoy very similar pay and T&CS to their colleagues in all other medical specialties.
Engaging with our members
The Faculty of Public Health will engage our members through regular updates via newsletters, webinars, and dedicated web pages outlining progress on parity of esteem. We will collaborate with our partners including the BMA and UKPHR on raising awareness of these issues and representing the voices of our member to policymakers. Interactive Q&A sessions and regional meetings will provide direct engagement opportunities on this and all other FPH related matters.
Professor Kevin Fenton, FPH President
Dr Ellis Friedman, FPH Registrar
Julian Ryder, Deputy CEX and Director of Education, Standards and Advocacy
March 2025

